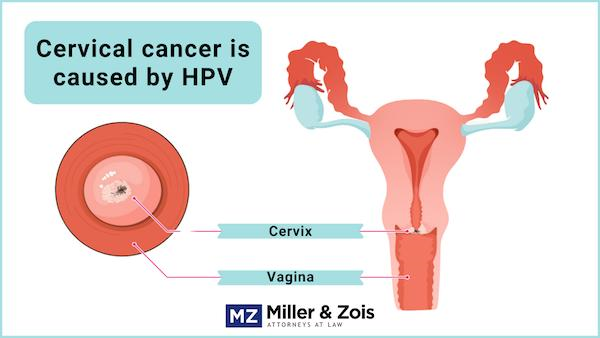
The cervix is a part of the female reproductive system. It is a narrow cylinder of tissue that connects the uterus and vagina. Cancer that originates in the cervix is known as cervical cancer.
Cancer is more successfully treated when it is diagnosed in its early stages. This is because cancer treatments are improving all the time. When a doctor fails to diagnose or misdiagnose cervical cancer, valuable time is lost.
If you or a loved one was the victim of cancer misdiagnosis, our medical malpractice lawyers may be able to help. We are experienced in cancer science and fighting insurance companies to get the best results for our clients. Contact us for a free consultation today by calling (800) 553-8082 or filling out our brief online form.
Below our lawyers outline cervical cancer, from those at risk to recent medical studies. If you have a specific area of interest, follow the links below.
In this article:
What is Cervical Cancer?
Cancer is a disease that happens when a genetic mutation causes cells to multiply uncontrollably. When this originates in the cervix, it is called cervical cancer. Almost always, this is caused by an HPV (human papillomavirus) infection.
The cervix has two parts lined with two different types of cells. The endocervix, or the opening of the uterus, is lined with glandular cells. The exocervix, also known as the ectocervix, is the outer part of the cervix and is lined with squamous cells.
“Cervical cancer originates in the cervix and can potentially spread to nearby and distant organs.”
This is important because cervical cancer most often begins in the areas where these two types of cells intersect, known as the transformation zone. Additionally, this cancer is classified based on which of these two cells become cancerous.
Most of the time, this cancer starts as a squamous cell carcinoma, beginning with the squamous cells. Other times, adenocarcinomas begin with the glandular cells. Rarely, the cancer begins in both cells, called an adenosquamous or mixed carcinoma.
Can Cervical Cancer Be Prevented?
If the cancer is a squamous cell carcinoma, which is almost always the case, it was almost certainly caused by HPV, the human papillomavirus. HPV is the most common sexually transmitted infection, affecting more than half of all sexually active people worldwide.
However, the types of high-risk HPV that can cause cervical cancer, types 16 and 18, are prevented by the HPV vaccine. People between the ages of 9 and 45 can get the vaccine. In the US, children routinely get the vaccine when they are 11-12. The HPV vaccine cannot, however, prevent the small percentage of cervical cancers that are adenocarcinomas or mixed carcinomas.
Cancer cells in the cervix develop gradually, meaning cervical cancer can be caught in its pre-cancerous stage. This is when the cells show signs of cancer but are not yet cancerous. Not all pre-cancers become cancer. Proactively treating a pre-cancer, though, will prevent any cancer from developing. Unlike other cancers that affect the female reproductive system, cervical pre-cancers can be detected by Pap tests (Pap smears).
The HPV vaccine and Pap tests significantly reduce the risk of cervical cancer. This is why cervical cancer mortality rates are far higher in regions where vaccinations and testing are unavailable.
Am I at Risk for Cervical Cancer?
Not having had the HPV vaccine and not getting routine Pap tests are the most significant risk factors for HPV. Several other factors may increase the risk of cervical cancer:
- HIV/AIDS or another condition that compromises the immune system
- Smoking/poor diet
- Being sexually active/pregnant at a young age
- Having many sexual partners
- Family history of cervical cancer
- Having three or more full-term pregnancies
What Are the Signs That I May Have Cervical Cancer?
Pre-cancerous or early-stage cervical cancers usually have no symptoms. Once the cancer begins to spread, the following symptoms may be experienced:
- Vaginal bleeding (after menopause, between periods, after sex, or abnormally heavy periods)
- Unusual vaginal discharge
- Painful sex
- Pain in the pelvic region
- Swollen legs
- Blood in urine, difficulty going to the bathroom
“The most important risk factors for cervical cancer are HPV and not regularly having Pap tests.”
How Is Cervical Cancer Diagnosed?
Pap tests are used during routine pelvic examinations to screen for cervical cancer. In a Pap test, or Pap smear, a gynecologist uses a speculum to widen the vaginal opening to collect a cell sample. The cells are then analyzed under a microscope to look for cancer cells. Doctors can do an HPV test at the same time.
Abnormalities found during routine pelvic exams and abnormal vaginal bleeding should cause a doctor to suspect cervical cancer and order further tests to confirm or rule out the condition.
“When a doctor does not properly diagnose cervical cancer, the patient may have a worse outcome due to that error.”
Doctors usually can diagnose cervical cancer with a Pap smear combined with a biopsy or the removal of a small piece of tissue. To take a biopsy, medical professionals will use a colposcope, a tiny magnifying glass inserted into the vagina to view the cervix.
Once cancer is diagnosed, doctors need to determine its stage. Staging is the process of determining how far the cancer has spread throughout the body. Doctors use X-rays, CT scans, and other tests to do so. Put simply, the stages of cervical cancer are:
- Pre-cancer: Abnormal cells exist but have not become cancerous
- Stage I: There is cancer in the cervix
- Stage II: There is cancer has spread to the uterus
- Stage III: The cancer has spread to the vagina or walls of the pelvis
- Stage IV: The cancer has spread to the bladder and other organs
How Is Cervical Cancer Treated?
In countries like the United States, cervical cancer is considered highly treatable due to the many prevention and early detection opportunities. When cervical cancer is not found in the early stages, sometimes due to misdiagnosis, treatment is more challenging and often less effective.
“Cervical cancer is often curable in the early stages but becomes harder to cure as it spreads.”
Treatment options depend mainly on where the cancer is located and the patient’s wishes. Early-stage cancers are treated with a biopsy to remove the cancerous tissue and lymph nodes. For women who do not wish to preserve their ability to have children, a hysterectomy, or the removal of the uterus and cervix, is another option.
The further the extent of the cancer, the greater the need for more extensive surgeries and, radiation therapy, and chemotherapy to kill the cancer cells.
Frequently Asked Questions
How deadly is cervical cancer?
The prognosis for cancer depends on what stage it is in when it is discovered and treated. According to the American Cancer Society, the 5-year survival rate for all women with this cancer is 66%. The rate changes dramatically by stage. For localized cancer, which has not spread, it becomes 92%. For regional cancer, which has spread to nearby lymph nodes, it decreases to 56%, for distant cancer, which has spread to distant organs, it drops to 17%. These figures show that early diagnosis is critical to living longer with this and most other cancers.
The HPV vaccine, invented by Australian scientists, first came to the US in 2006. Between 2008 and 2014, the percentage of pre-cancers caused by HPV types 16 and 18 (the most common cause of cervical cancer) dropped by 8.6%. This statistic includes women who did not receive the vaccine, suggesting that its pervasiveness in the human population will continue to weaken as the vaccine continues to be used.
How common is cervical cancer?
Cervical cancer is the fourth most common cancer in women (other common cancers include skin cancer, breast cancer, and lung cancer). It affects around 8 out of every 100,000 women in the United States. In 2018, there were 570,000 cases of this cancer worldwide, along with 311,000 deaths. 90% of these deaths occurred in low- to middle-income countries, and experts say that a scaling up of vaccines, screening, treatment, and social mobilization is required to correct this imbalance.
Though it is still possible to have cervical cancer at a young or older age, most cervical cancer is diagnosed in middle-aged women between the ages of 35 and 44. In the United States, Hispanic women are the most likely to get this cancer, while Asian and Pacific Islanders and American Indians are the least likely to get the disease.
What causes misdiagnosis?
Misdiagnosing cancer is a costly mistake and may constitute malpractice or wrongful death. Any delay in diagnosis subsequently causes a delay in treatment, allowing the cancer to spread unchecked. This could mean that a cancer patient will need more invasive surgeries or even have a reduced life expectancy than if they had been diagnosed when they should have. Cancer misdiagnosis can happen for many reasons.
First, if a woman presents to a healthcare professional with any of the symptoms of ovarian cancer (unusual discharge, pain, etc.), that doctor needs to perform testing or refer the patient for testing. The doctor should thoroughly investigate the patient and ask detailed questions about their history.
Diagnostic errors do not always lie with the doctor. The error may lie with the lab technician who interpreted the Pap smear test results. Or, there may have been an error in the communication between the healthcare facility and the laboratory. It is also a problem if the doctor fails to communicate with and inform the patient about what is going on.
Failure to timely diagnose cervical cancer can lead to severe pain and suffering, the loss of reproductive organs, premature death, expensive treatment, and an increased time to recovery for the plaintiff.
Is misdiagnosis medical malpractice?
Failure to recognize and diagnose cervical cancer can lead to severe pain and suffering, the loss of reproductive organs, premature death, expensive treatment, and an increased time to recovery. The plaintiff may be able to “recover” these consequences in the form of monetary damages in a medical malpractice lawsuit or wrongful death lawsuit.
This is not necessarily malpractice if a patient is treated for their cancer and the treatment is unsuccessful. For malpractice to have occurred, there must have been an oversight or error in diagnosis or treatment that does not live up to the standards of medical care that doctors are required to follow. This includes failing to recognize or investigate symptoms, correctly analyzing a cancer test’s results, and other errors.
Sample Cervical Cancer Settlement Amounts and Jury Payouts
- 2019, Pennsylvania: $9,680,000 Verdict The plaintiff, a minor, visited several doctors over two years with complaints of irregular periods. She underwent an ultrasound that revealed a cervical mass. Doctors failed to notify her family and to refer her for treatment. Two months later, she was brought to the emergency room, where staff notified her family of the mass. One month later, she was diagnosed with Stage III cervical cancer and underwent radical, disabling surgery. Her family sued the doctors for failing to diagnose it promptly. A jury awarded the plaintiff and her family $9,680,000.
- 2019, Massachusetts: $1,000,000 Settlement The plaintiff, a woman, went to her primary care doctor complaining of vaginal bleeding between her periods. The plaintiff told the physician that she had been bleeding like this for over a year. The plaintiff alleges that even though her Pap test was abnormal, the physician failed to note the result or notify her. She is diagnosed a year later at the hospital with metastatic cancer. The defendant denied liability but settled with the plaintiff for $1 million before trial.
- 2017, California: $1,900,000 Settlement The plaintiff is a 39-year-old woman who underwent a Pap smear and an HPV test that showed abnormal results. Her gynecologist recommended a colposcopy. However, the gynecologist failed to announce her test results. The plaintiff visited the same gynecologist less than a year later, complaining of bleeding and abdominal cramps. She was prescribed birth control pills. The following year, her gynecologist announced that she suffered from fibroids and her steroid use caused bleeding. She underwent fibroid surgery, where she was revealed to have Stage IV cervical cancer. The plaintiff died the following year. Her husband sued the gynecologist, alleging delays in his late wife’s cervical cancer diagnosis. He also alleged that the pathologist misinterpreted her tissue samples. The case settled for $1,900,000.
Recent Medical Studies
- Three large-scale surveys highlight the complexity of cervical cancer under-screening among women 45–65 in the United States by Diane Harper et al., Preventative Medicine, Jan. 2020.
Increasing the screening rate is one of the steps needed to eliminate cervical cancer worldwide—a technically possible goal. With that in mind, the researchers in this study looked at data from three extensive studies in the US on cervical cancer screening in older women ages 45-65. They note the demographic factors influencing the screening rate, including geographic location, race, and economic status. The authors conclude that the current screening rate is insufficient to eliminate cervical cancer in this population. - Exacerbating disparities?: Cervical cancer screening and HPV vaccination by Michelle Silver and Sarah Kobrin, Preventative Medicine, Jan. 2020.
Also, using some of the national data that the above study utilized, this study analyzed the link between having an HPV vaccination and getting screened for cervical cancer in American women. They found that only 27% of women who could get the vaccine had it. Women who had gotten the vaccine were also more likely to get screened. Young women and uninsured women were less likely to do either of these things. - A Novel Technique to Minimize Contamination for Cervical Cancer Surgery Patients by Martin Martino et al., Journal of Minimally Invasive Gynecology, Jan. 2020.
Surgeons can use a minimally invasive technique to perform surgeries on cervical cancer patients. This technique uses a laparoscope tool, so the doctor does not have to cut through the skin to operate. Instead they view the inside of the body with a camera and operate with long tools inserted into the abdomen. Researchers discovered that laparoscopy in women after hysterectomy for cervical cancer had higher relapse rates and lower survival rates than open surgery. Researchers suggest a new technique in this new study that may solve that issue.
More Information
- Cancer misdiagnosis overview
- Medical malpractice overview
- Wrongful death lawsuits
Contact Us
If you or a family member suffered due to the misdiagnosis of cancer, our medical malpractice lawyers may be able to help you. This is a difficult time for your family, and our lawyers are here to help you get the monetary compensation you need and deserve.
For a free consultation of your potential medical malpractice case, call our Maryland medical malpractice lawyers at (800) 553-8082 or fill out our brief online form.
 Medical Malpractice
Medical Malpractice





